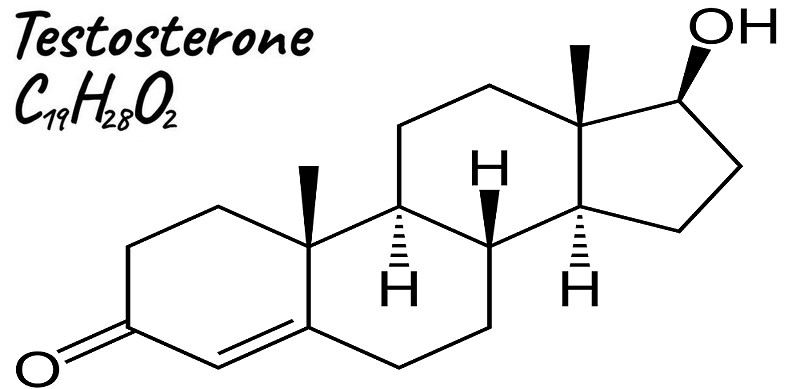
Testosterone
Part 1: What it is and how it is made
By Joachim Bartoll, May/June 2015, for Classic Muscle Newsletter, issue 10
Testosterone is a 19-carbon steroid hormone belonging to the androgen group. It’s made from cholesterol (like all sex hormones) and its immediate precursor is DHEA. On average, a healthy man’s body will produce about 7 mg of testosterone a day, but not all of that Testosterone can be used by our bodies. While our total testosterone can be high, we might still be experiencing symptoms of low testosterone. To make sense of this, we need to look at the three sub-types of testosterone:
1. Free testosterone. This is the real deal, it’s testosterone in its purest form. It’s called “free” because there aren’t any proteins attached to it. Only the free form of testosterone can enter cells where it activates certain receptors in order to work its magic on our bodies and mind.
Free testosterone makes up only 1 to 4 percent of our total testosterone levels. So, it’s quite clear that you want to have as much free testosterone in your bloodstream as possible.
2. SHBG-bound Testosterone. About 60 to 70 percent of our total testosterone is bound to a protein called sex hormone-binding-globulin (SHBG), which in men also is called testosterone-binding globulin. SHBG is produced in our livers and plays an important role in regulating the amount of free testosterone in our bodies. Once testosterone is bound to SHBG it becomes biologically inactive, meaning that our bodies no longer can use it to build muscle or boost our mood. SHBG in itself isn’t bad and is needed to balance our hormones. But too much SHBG can cause problems since it lowers our amount of free testosterone. This is why it’s possible to have high total testosterone levels, but still suffer symptoms of testosterone deficiency.
3. Albumin-bound Testosterone. The rest of our testosterone (30 to 40 percent) is bound to a protein called albumin. Albumin is the main protein of human blood plasma, and its job is to stabilize extra-cellular fluid volumes (the osmotic pressure of blood). Like SHBG-bound testosterone, albumin-bound testosterone is biologically inactive. There is one important difference though; unlike Testosterone bound to SHBG, the bond between albumin and testosterone is weak and can be easily broken in order to create free testosterone “when needed”, as regulated by our hypothalamus. Therefore, the term bioavailable testosterone (BAT) refers to the sum of free testosterone plus albumin-bound testosterone (even if this is not exactly correct). Some labs actually lump albumin-bound testosterone together with free testosterone when you get tested, which is not really relevant. Always ask for exact measures of all three forms of testosterone.
While bound testosterone works like a reserve and must be released from its bond to be utilized, your free form of testosterone is constantly being used by your body. The more testosterone available in its free form, the more noticeable is testosterone’s effect on the body.
While you will experience bursts in free testosterone from, for example, intense exercise, these spikes in free testosterone are both small and short lived, and the impact is therefore almost negligible.
To notice an effect from a temporarily boost in testosterone, it has to be significant and last for several hours. An example of this would be the casual steroid user taking only one daily dose of the oral Dianabol, which has a half-life of 3 to 5 hours, and will produce varying blood levels with ups and downs throughout the day (up to 10 hours).
The roles of testosterone
The group of male hormones that create and support masculinity is known as androgens (also called androgenic hormones or testoids). The primary androgen is testosterone, other androgens include Dihydrotestosterone (DHT), Dehydroepiandrosterone (DHEA) and androstenedione (Andro). While these are less known, they are of equal importance in male development.
Looking at testosterone, the hormone is primarily responsible for:
- Determining the sex of a child before birth
- Influencing sexual preferences
- Forming personalities
- Regulating the sex drive in both men and women
- The development of male sexual characteristics including dominance, emotional and physical strength, body shape, hairiness, deep voice, and odor
- Governing sperm production and quality
- The ability to perform adequately during sexual intercourse
- The development of the nervous system and the ability to recruit fast twitch muscle fibers
Testosterone also plays a role in developing creativity, intellect, thought patterns, sense of pride, honesty, assertiveness and drive, as well as the ability to propose new ideas and carry them through to successful conclusions.
Testosterone also affects general health during childhood, adolescence and adulthood. Sufficient levels of testosterone help males to thrive as children and to develop stronger muscles and bones. Adequate testosterone levels during adulthood are crucial for your energy levels, keeping optimistic and coping with stress and negativity. As you grow older, keeping your testosterone levels as high as possible is key to aging gracefully and enjoying life.
Symptoms of declining testosterone levels include decreased sex drive, erectile dysfunction, impaired fertility, testicular shrinkage, loss of body hair and muscle mass, depressed mood, irritability, lack of energy and decreased metabolism, hot flashes, and difficulties with concentration and memory. Men with low testosterone may also experience weight gain, breast enlargement, decreased bone density, and problems urinating.
How testosterone is made
Testosterone is produced mainly in the testes in males (more than 95 percent) and in the ovaries in females. A small amount is made in the outer layer of the adrenal glands in both sexes. The process that carefully regulates the amount and timing of testosterone production is complex and begins in the brain. It can be broken down in the following steps:
1. When our hypothalamus detects that our body needs more testosterone, it secretes a hormone called gonadotropin-releasing hormone (GnRH). The gonadotropin-releasing hormone makes its way over to the pituitary gland in the back of our brain, where it causes the gland to produce two other hormones; follicle-stimulating hormone (FSH) and luteinizing hormone (LH), collectively known as gonadotropins.
2. LH and FSH is released into the bloodstream where they travel to the male testes. FSH stimulates sperm production while LH triggers the production of testosterone from cholesterol. Once the levels of testosterone have increased, the pituitary slows the release of LH so production slows down. This is known as a negative feedback loop.
3. When the small amount of newly produced testosterone is released into the bloodstream, most of it immediately attaches itself to SHBG and albumin, thus becoming biologically inert. Only a tiny amount remains free and can move from the blood stream into cells where it is needed.
With such a complex chain of events during the production of testosterone, many problems or interruptions can occur, leading to sub-normal or low testosterone levels. If there are any negative conditions (or diseases) involving the male testes, hypothalamus, pituitary gland or genetic material, the production of testosterone is severely hampered, and the resulting state is called hypogonadism.
It’s also important to understand that your testosterone levels are usually at their highest in the morning and slowly fall during the day to reach their lowest in the evening.
In the next part we’re going to look closer at the benefits of optimal testosterone levels, common causes for low testosterone levels and ways to increase our free testosterone.
Reference values
TESTOSTERONE, TOTAL
Males
0-5 months: 75-400 ng/dL
6 months-9 years: <7-20 ng/dL
10-11 years: <7-130 ng/dL
12-13 years: <7-800 ng/dL
14 years: <7-1,200 ng/dL
15-16 years: 100-1,200 ng/dL
17-18 years: 300-1,200 ng/dL
> or = 19 years: 240-950 ng/dL
Females
0-5 months: 20-80 ng/dL
6 months-9 years: <7-20 ng/dL
10-11 years: <7-44 ng/dL
12-16 years: <7-75 ng/dL
17-18 years: 20-75 ng/dL
> or =19 years: 8-60 ng/dL
TESTOSTERONE, FREE
Males: 9-30 ng/dL
Females: 0.3-1.9 ng/dL
Reference values have not been established for patients that are less than 16 years of age.
TESTOSTERONE, BIOAVAILABLE
Males
< or =19 years: not established
20-29 years: 83-257 ng/dL
30-39 years: 72-235 ng/dL
40-49 years: 61-213 ng/dL
50-59 years: 50-190 ng/dL
60-69 years: 40-168 ng/dL
> or =70 years: not established
Females (non-oophorectomized)
< or =19 years: not established
20-50 years (on oral estrogen): 0.8-4.0 ng/dL
20-50 years (not on oral estrogen): 0.8-10 ng/dL
>50 years: not established